Abstract
Background
Chronic myeloid leukemia (CML) diagnosed during pregnancy is a rare situation with no standard treatment schemes. If a pregnancy is prolonged weighting the risks/benefits of therapy or observation without therapy is a complicated task. If a pregnancy is terminated a possibility of a further childbirth has to be judged. The course of the disease, treatment options and possible outcomes need to be known in these patients (pts) in the era of tyrosine kinase inhibitors (TKIs).
Aim To describe pregnancy outcomes, therapy and follow-up in women with CML diagnosed during pregnancy in the era of TKIs
Methods
We made a search in the databases of pregnancy cases in CML pts after 2003 year, since the first TKI imatinib became available. The data were obtained from observational studies: CML pregnancy registries of Russian hematology society and ELN. Clinical and demographic characteristics of pts, therapy, monitoring, pregnancy outcomes and follow-up were analyzed.
Results. We found that 48 of 199 women with CML and pregnancy were diagnosed as having CML during pregnancy in years 2006-2018. Median (Me) age at CML diagnosis was 26 years (range 19-39). All pts had a chronic phase of CML. Sokal score was low in 34(71%), intermediate in 9(19%) high in 4(8%) and not known in 1(2%) pt. CML was diagnosed during 1st, 2ndand 3rd trimester of pregnancy in 26(54%), 11(23%) and 11(23%) females, respectively.
Elective abortion was done in 14 (29%) pts, 1(2%) pt had a miscarriage. All 15 pts started TKI therapy shortly after delivery. Me observation time after labour was 52 months (range 4-139). Imatinib (IM) and nilotinib (NIL) were used as 1st line therapy in 14 and 1 pt accordingly. Five pts were switched from IM to a second line TKI due to resistance in 3 pts and to physician choice in 2 pts. Deep molecular response (DMR or BCR-ABL≤0,01% IS) and major molecular response (MMR or BCR-ABL≤0,1% IS) was achieved in 6 and 5 pts. No molecular response 2 (MR2 or BCR-ABL≤1%) was reported in 4 pts with the follow-up of 24-184 months. One pt died due to CML progression in BC (resistant to IM, T315I mutation, relapsed after allogenic bone marrow transplant (BMT), pre ponatinib availability).
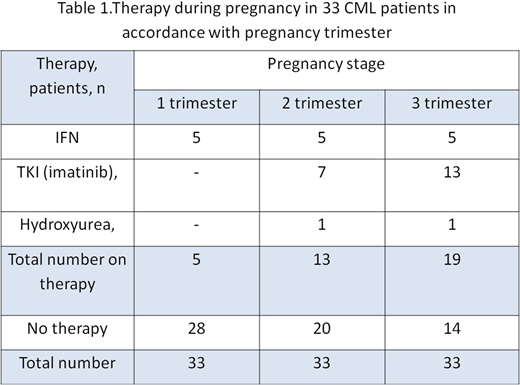
Pregnancy was carried out in 33(71%) pts: in 11 of 26 pts with CML diagnosed at 1st trimester and in all 22 pts diagnosed at 2nd-3rd trimester. Pregnancy ended in labour in 32 pts while in 1 pt pregnancy was ongoing pregnancy (week 26th) at the time of evaluation. No therapy for whole pregnancy was in 14 pts: 1, 5 and 8 of them were diagnosed in 1st, 2nd and 3rd trimester accordingly. Therapy during pregnancy was started in 19 pts: 10, 6 and 3 pts with CML diagnosed in 1st, 2nd and 3rd trimester accordingly. Five pts got interferon (IFN) in 1st trimester and 3 of 5 were switched to IM in 2nd-3rd trimester. Four pts got hydroxyurea (HU) for 5-7 days in 1st-2nd trimester prior to any other therapy. Fourteen pts with no therapy in 1st trimester started therapy at late pregnancy: IM since 2nd-3rd trimester in 10 pts, HU in 3rd trimester in 1 pt. A total of 13 pts got IM with Me time of IM start at 18 weeks (range 16-35). Me time of observation after delivery was 52 months (range 4-139). Me time of delay in TKI administration after diagnosis was 7 weeks (range 1-51) and in total 12(36%) of 33 pts got IFN or HU before TKI. TKIs used as 1st line were as follows: IM, dasatinib and NIL in 30, 1 and 1 pts accordingly. Nine pts were further switched from IM to TKI2 as 2nd line due to resistance/suboptimal response. DMR and MMR was achieved in 11 and 17 pts accordingly, MR2 in 5 pts, no MR2 in 1 pt with short follow-up (4 months), 4 pts were too early to evaluate. Two pts were resistant to 2 lines of TKIs and died from disease progression; one of them had a BMT failure and 1 pt was non-compliant.
Thirty three children were born (one twins): 17 boys and 16 girls, no births defects were observed. Seven newborns had a low birth weight (<2500g): 6 of them were exposed to IM at late pregnancy and 3 were born preterm at week 35-37. Follow-up of the children was uneventful.
Eleven pts later had 13 pregnancies which ended in childbirth within Me 5 years (1-9 years)
Conclusion
CML may be diagnosed at any pregnancy stage and pregnancy termination/prolongation should be judged individually. A normal childbirth may take place including cases with use of IM at late pregnancy. It is reasonable to adjust therapy options to pregnancy trimester and to avoid potential teratogenic drugs at 1st trimester. A careful follow-up and timely monitoring of these cases is needed.
Chelysheva:Fusion Pharma: Other: provided consultations ; Bristol Myers Squibb: Other: provided consultations and performed lectures; Novartis: Other: provided consultations and performed lectures. Abruzzese:Pfizer: Consultancy; BMS: Consultancy; Novartis: Consultancy; Ariad: Consultancy. Rea:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Incyte: Honoraria; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria. Kim:BMS: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Ilyang: Research Funding. Chabaeva:Russian Foundation for Basic Research grant 18-015-00399 A: Research Funding. Kulikov:Russian Foundation for Basic Research grant 18-015-00399 A: Research Funding. Turkina:Novartis: Other: provided consultations; Bristol Myers Squibb: Other: provided consultations; Phizer: Other: provided consultations; Fusion Pharma: Other: provided consultations.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal